Stop the Revenue Leak in Healthcare System
Hospitals lose revenue to denials, delays, and manual work. We help teams recover faster, reduce repeats, and keep staff focused on care - not paperwork.

Leaks Hospitals Can’t Ignore
Denied at First Submission
Nearly 1 in 6 claims are rejected, delaying payment and adding cost
Revenue Lost to Leakage
Missed charges, coding errors, and system gaps drain millions
Lost to Underpayments
Contract shortfalls & hidden discrepancies reduce net revenue
Solving Revenue Cycle Challenges for Healthcare Industry
Neuriphy eliminates inefficiencies in medical billing through advanced AI technology. We transform complex revenue workflows into streamlined, intelligent processes.
Automate critical financial tasks
Protect hospital revenue streams
Reduce operational complexity

One Engine, Many Wins
Behind every feature is the same foundation: a platform that connects smoothly, grows with you, and keeps getting smarter.

Seamless Integration
Neuriphy connects smoothly with EHRs, clearinghouses, and payer portals without disrupting workflows. Secure data exchange cuts manual steps, keeps systems in sync, and ensures claims move faster from submission through resolution.
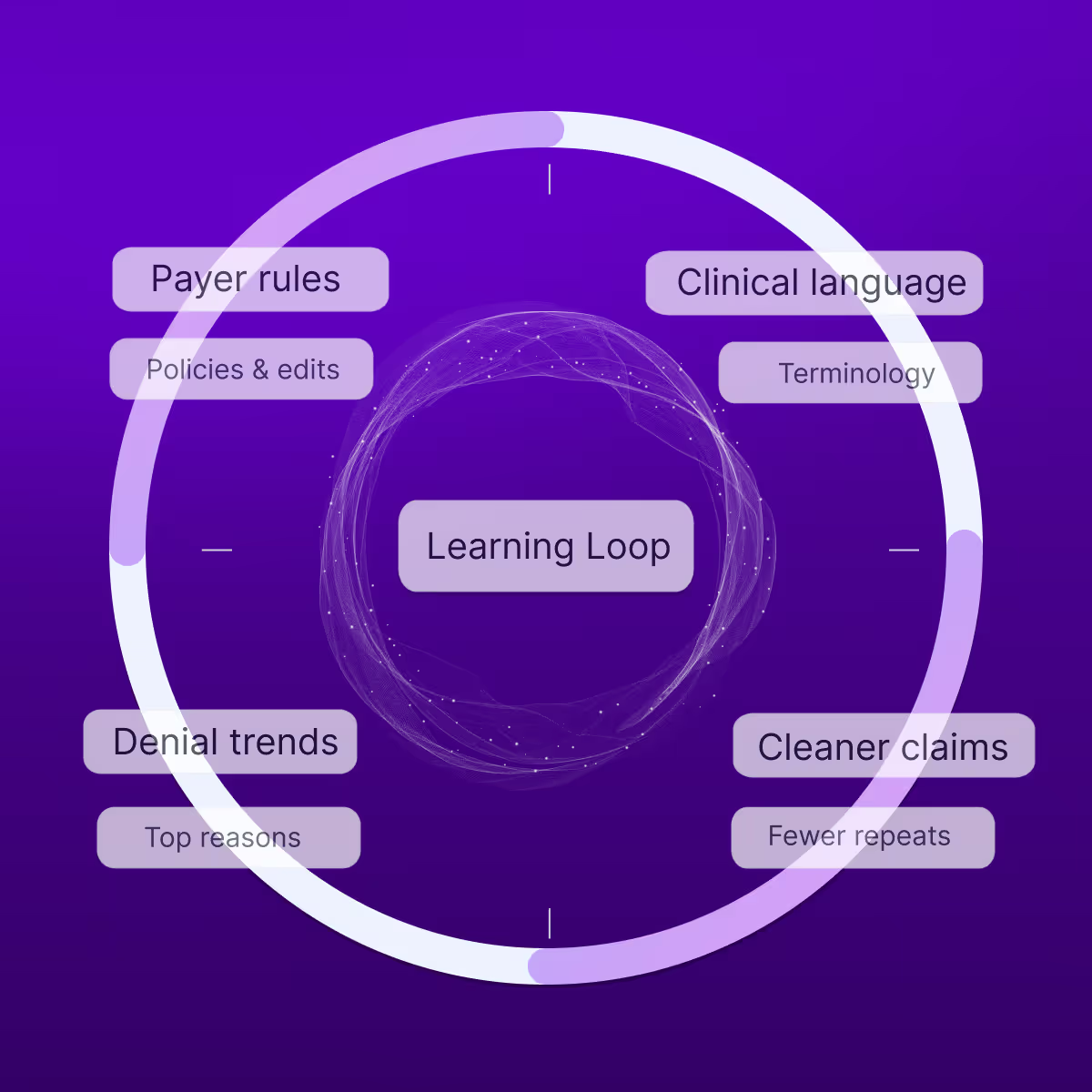
Continuous Learning
Neuriphy adapts with every claim it processes. By learning from payer rules, denial trends, and clinical language, it gets smarter over time, improving accuracy, reducing repeat issues, and helping your revenue cycle stay ahead.

Dynamic Expansion
Built to handle growth, Neuriphy scales effortlessly across facilities, specialties, and payers. Whether processing thousands or millions of claims, performance stays reliable so your team can expand operations without extra staff or costly upgrades.
Improving Healthcare Financial Outcomes
Revenue Acceleration
Achieve 1.5–3% net revenue lift annually by capturing missed charges and overturning denials effectively.
Faster Payment Cycles
Accelerate reimbursements by automating denial workflows, eligibility checks, and appeal submissions to reduce A/R days.
Lower Operating Costs
Cut expenses by automating manual claim tasks, reducing reliance on large back-office administrative teams.
System-Wide Scalability
Integrate across fragmented EHRs, clearinghouses, and payer portals without new infrastructure while ensuring full compliance.
Higher Staff Productivity
Eliminate repetitive claim handling tasks so staff can focus on strategic, high-value financial initiatives.
Improved Work Quality
Reduce errors with automated reconciliation, coding precision, and compliant appeal generation for consistent accuracy.
Continuous improvement
Implement iterative learning mechanisms that continuously refine and enhance revenue capture methodologies.
Stronger Oversight
Enable leadership with dashboards that track denials, recovery trends, and payer compliance in real time.
How It Works
Neuriphy plugs into your revenue cycle and quietly takes over the heavy lifting. From intake to recovery, every step is automated, tracked, and secured.
Connect
Creates a secure link with EHRs, clearinghouses, and payer portals while keeping existing workflows intact.
Analyze
Continuously reviews claims, codes, and payer rules to identify risks, errors, and missed opportunities in real time.
Prioritize
Ranks issues by financial impact and urgency, assigning clear worklists so staff focus on what matters most.
Improve
Validates documentation, generates compliant responses, and resubmits claims quickly to secure payments.
Accelerate Your Revenue Potential
Break free from traditional revenue cycle limitations. Partner with Neuriphy and transform financial performance through intelligent, data-driven solutions.