Autonomous Revenue Cycle Platform for Healthcare
An AI-driven platform built for hospitals and healthcare providers, transforming revenue management by preventing claim denials and recovering lost revenue through intelligent automation.

Challenges Blocking Revenue Performance
Hospitals are losing revenue to first-pass denials, hidden underpayments, and slow, manual follow-ups. Data lived in silos, payer rules kept shifting, and teams couldn’t scale prevention.
Manual Work
Hours spent gathering documentation, checking portals, and drafting letters don’t scale as volumes grow and complexity increases.
Reduce Manual Tasks
Financial Clearance
Automate repetitive tasks, reducing staff time by up to 60%. Auto-verify coverage benefits up front.
High First-Pass Denials
10–15% of claims fail first submission, creating rework, write-offs, appeal backlogs, and avoidable revenue leakage systemwide.
Improve Denials
Denials Management
Our LLM-Powered Solution improve denials overturn rates by up to 30-40% & accelerate Cash Flow.
Hidden Underpayments
Small variances across contracts, modifiers, bundles, and carve-outs escape reviews, quietly compounding into millions in losses.
Cut Underpayments
Underpayments
Capture underpayments that would otherwise go unnoticed with Intelligent Underpayment Identification
Change in Payer Rules
Frequent policy changes and payer-specific nuances cause inconsistency, compliance risk, and uneven results across facilities and specialties.
Recover Lost Revenue
Appeals Management
Improve the success of appeals by 25-30% compared to manual workflows
Proprietary LLM for Healthcare Revenue
Unlike generic AI, Neuriphy’s model is purpose-built for healthcare revenue cycle operations, trained on healthcare data such as claims, denials, remittances, and payer rules – delivering unmatched accuracy.
Key Capabilities that Power Neuriphy
Imagine a revenue cycle expert who has read every claim, every denial letter, every payer policy, and never forgets a single detail.
Thinks Like a Revenue Integrity Team
Detects missing charges, underpayments, and documentation gaps.
Learns From Every Claim
Adapts instantly to payer rule changes and evolving denials patterns.
Root Cause Analysis
Explains denial patterns and payer-specific nuances in plain language.
Payer Rule Adaptation
Continuously learns from payer policy changes and adjudication patterns.
Explains its Decisions
Transparent recommendations for compliance and audit readiness
Medical Necessity Validation
Evaluates claims and documentation to ensure services meet payer medical necessity criteria, reducing denials and rework.
Connect without Disruption
Plug into EHRs, clearinghouses, and payer portals. Keep current workflows intact.

EHR Integration
Integrates with EHRs, clearinghouses, and payers using secure FHIR, API, and EDI, ensuring smooth interoperability.
Clearinghouse Sync
synchronizes with clearinghouses to streamline claims submission and payer transactions.
Payer Portal
Connect directly with payer portals to streamline eligibility checks, authorizations, and claim status updates securely.
Compliance Framework
Built with HIPAA and SOC 2 standards, ensuring secure data handling and regulatory alignment across workflows.
Security and Compliance
You Can Trust
Proven controls and audit-ready practices keep operations safe while sustaining high performance.
Core Security Frameworks
HIPAA Compliance
SOC 2 Type II Controls
ISO Alignment
CMS Regulations




Data Protection & Privacy
End-to-End Encryption
Audit Trails
Secure Data Storage



Integration & System Trust
Secure Integration
FHIR, API, EDI, X12 Standards


Healthcare-Grade Security

Explore our Trust Center

Neuriphy’s Trust Center provides real-time visibility into our security and compliance posture, validated through continuous security and compliance posture, validated through continuous monitoring.
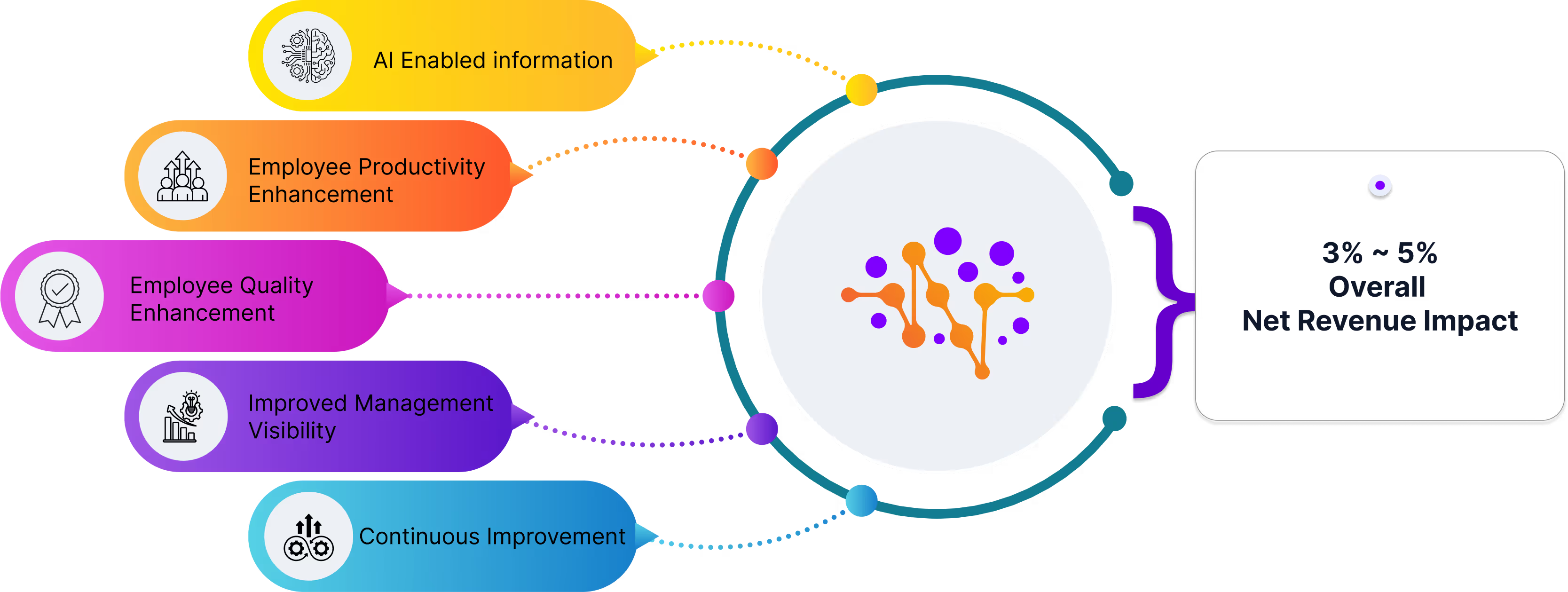
Comprehensive Platform Advantages
Transformative solutions for healthcare revenue management
Measurable Financial Impact
Predictable and sustainable revenue growth strategies.
Scalable Integration
Flexible platform adapts to diverse healthcare environments.
Compliance and Security
Robust protection of sensitive healthcare financial data.
Continuous Learning and Adaptation
Trained on healthcare data, Neuriphy’s platform brings measurable gains in revenue recovery, denial prevention, and operational efficiency.
Set to Redefine Healthcare Revenue?
Break free from revenue cycle complexity with an AI solution that understands the nuanced challenges of healthcare billing. Our platform turns financial obstacles into strategic opportunities.