Unlock Revenue Recovery with Our Proprietary LLM
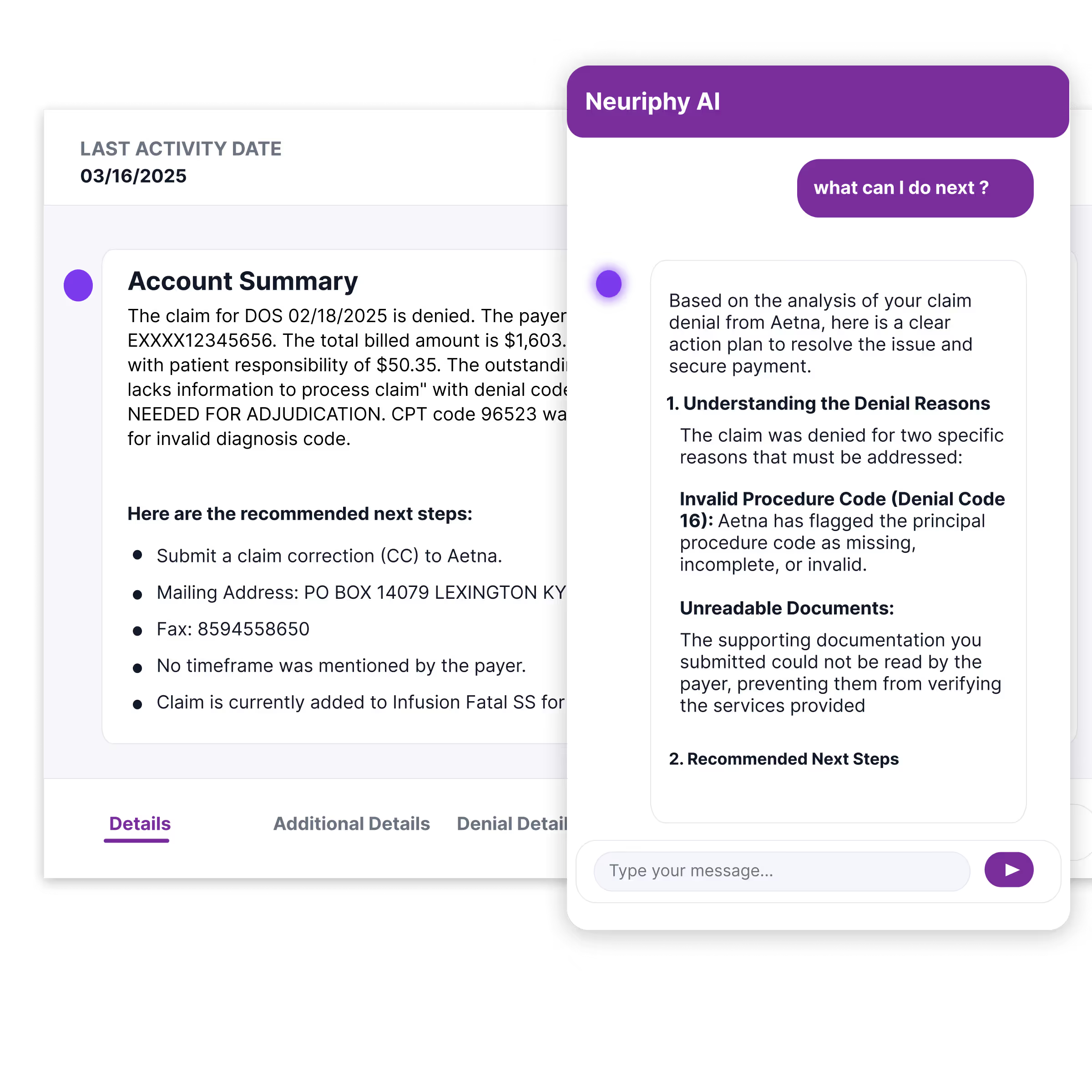
Neuriphy’s AI-powered denial management solution automates classification, prioritization, and appeals to cut A/R delays, reduce costs, and recover revenue faster.
Denial Backlogs: How They Happen
Excessive Administrative Burden: Hours per claim on documentation, portals, and letter drafting drain capacity.
Inconsistent outcomes: Results swing with payer nuance, human error, and incomplete data.
Revenue delays: Denials extend days in A/R and put real pressure on cash flow.
Low visibility: Limited root-cause insight keeps prevention efforts scattered and slow
Automated Denial Classification
Automatically interpret denial codes and EOBs, classifying claims by type, financial impact, and payer rules to streamline workflows and ensure accurate routing.
Code Interpretation: Read and understand payer denial codes at scale.
Impact-Based Sorting: Prioritize claims by financial value and urgency.
Payer-Specific Rules: Apply logic unique to each payer automatically.
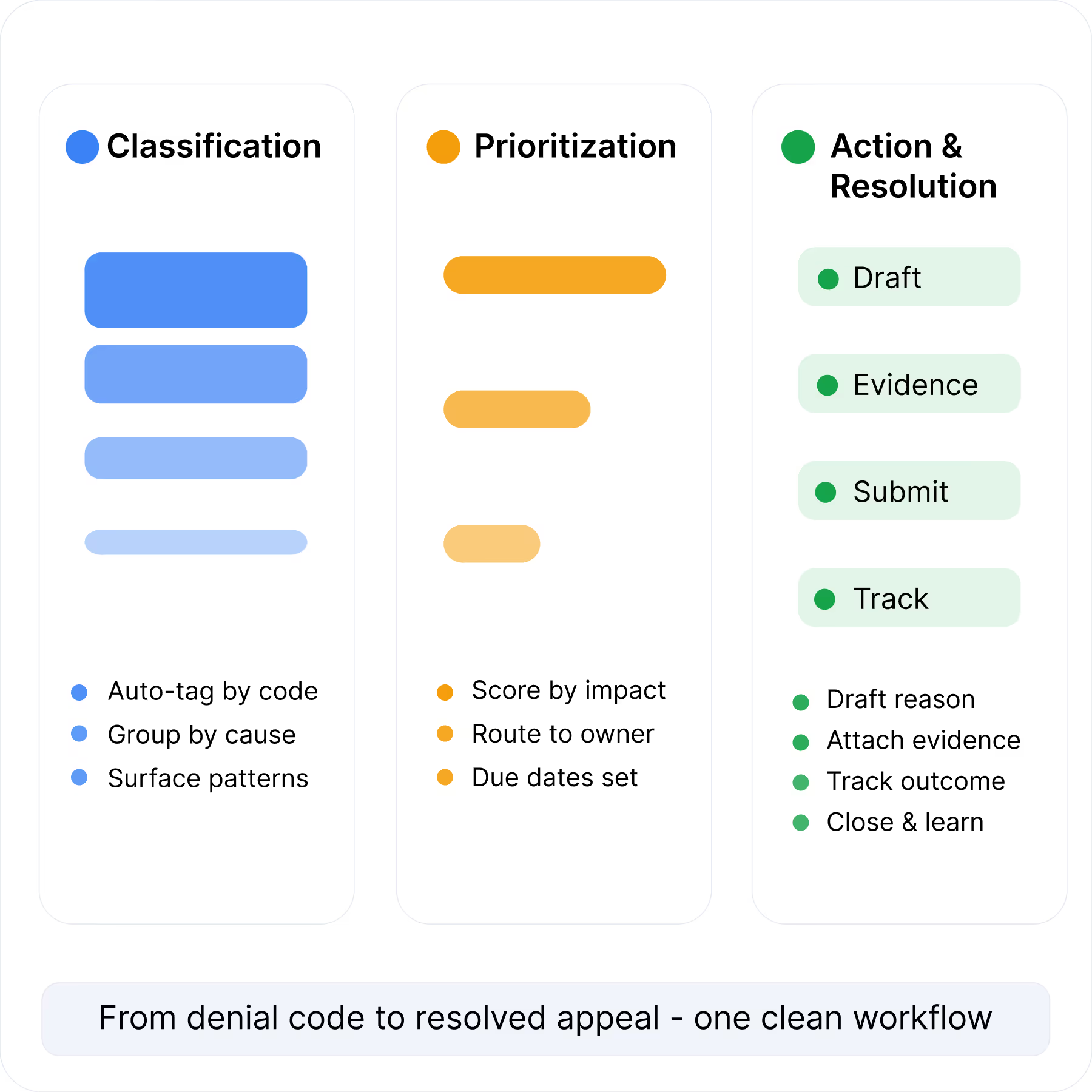
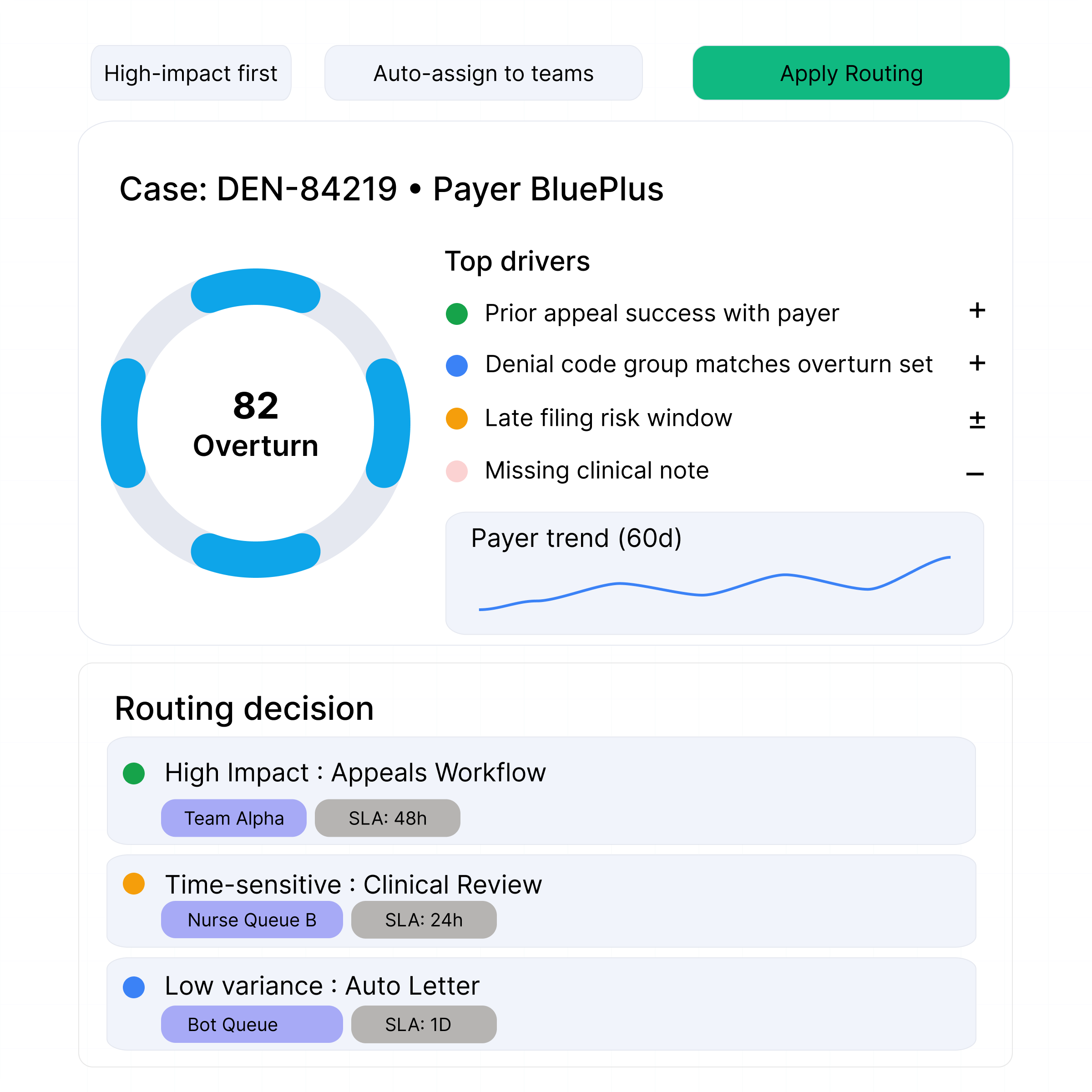
Smart Prioritization & Routing
Predict overturn likelihood using claim history, payer trends, and denial patterns, routing cases to the right workflow or team for faster resolution.
Overturn Prediction: Identify denials with the highest chance of success.
Automated Routing: Direct cases to the right specialists instantly.
Faster Recovery: Focus staff time on high-value, winnable denials.
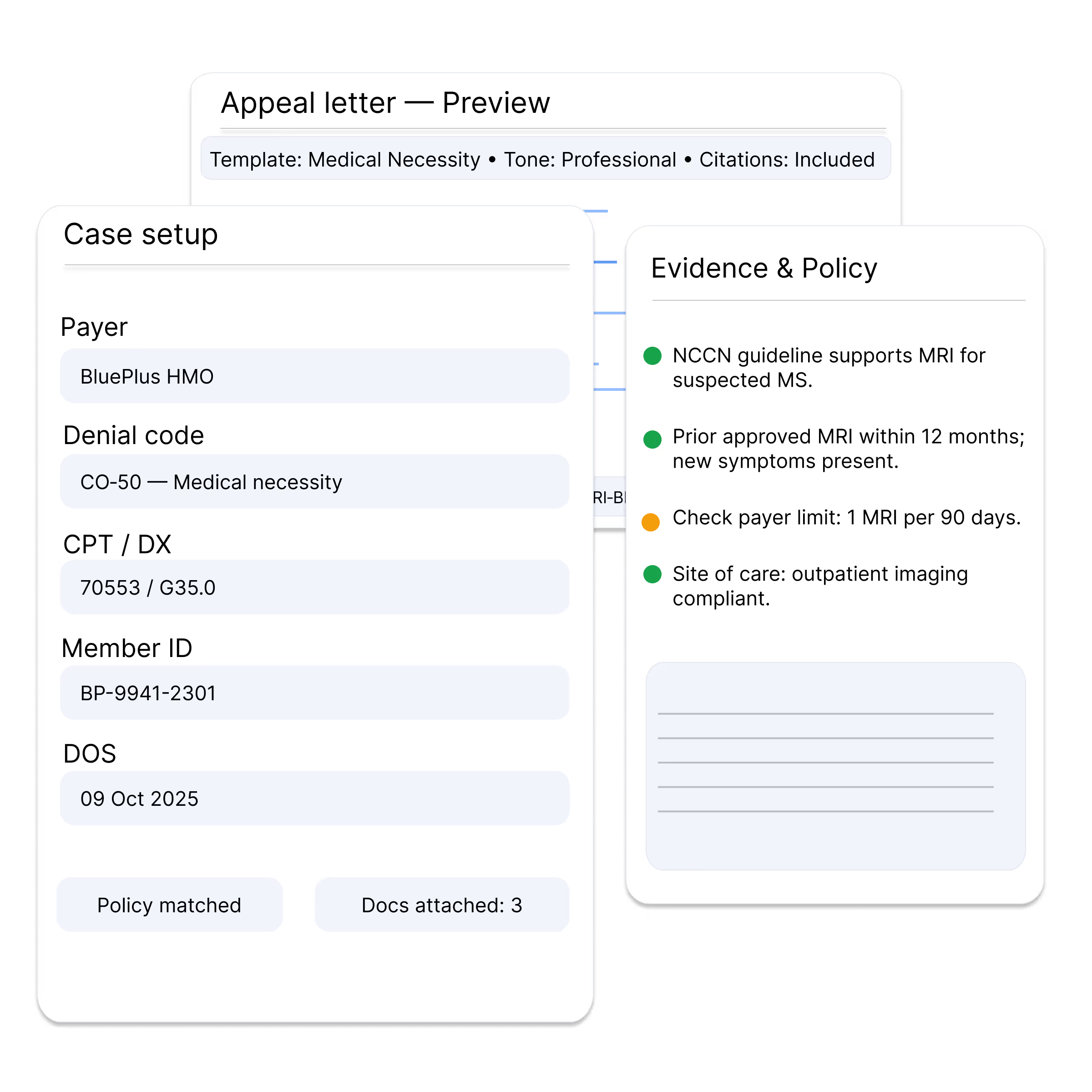
LLM-Powered Appeals Generation
Instantly generate payer-specific, evidence-based appeal letters that align with clinical documentation and regulatory criteria, improving overturn rates while reducing manual burden.
Automated Drafting: Create customized, compliant letters in minutes.
Evidence-Backed: Leverage clinical data and coding rules seamlessly.
Continuous Learning: Adapt appeal strategies based on payer responses.
Predictive Denial Prevention
Identify root causes such as missing documentation or coding errors, offering proactive recommendations to prevent repeat denials before claims are submitted.
Root-Cause Detection: Pinpoint recurring denial drivers.
Flag issues before claims reach payers.
Eliminate repetitive denials with proactive fixes.
Real-time Insights that Reveal Hidden Revenue Opportunities
Access dashboards that track denial volumes, payer behavior, overturn rates, and financial risk, with customizable reports for executives and compliance teams.
Performance Dashboards: Monitor trends and outcomes in real time.
Payer Analytics: Identify payer-specific denial patterns.
Custom Reports: Support compliance and financial oversight.
What Sets Our System Apart
What differentiates our system is its foundation on a proprietary large language model tailored for healthcare revenue cycle management, setting it apart from standard AI tools.
Domain-Specific Training: Trained on payer policies, denial codes, and healthcare documentation, not just general text.
Continuous Learning: Adapts to evolving payer rules and regulatory updates.
Context-Aware Intelligence: Understands both clinical and financial language, bridging the gap between coding, compliance, and revenue cycle.
Benefits of Smarter Denial Management
Automated denial management reduces financial loss by preventing repeat errors, improving overturn rates, and enabling smarter prioritization that saves staff time and accelerates reimbursement.
Fewer Denials
Automation minimizes manual claim handling, freeing staff to focus on strategic revenue tasks instead of repetitive workflows.
Accelerate Cash Flow
Smart prioritization and automated appeals generation shorten A/R cycles and accelerate cash recovery.
Cut Administrative Costs
Automation minimizes manual claim handling, freeing staff to focus on strategic revenue tasks instead of repetitive workflows.
Modernize Your Revenue Cycle Now
Harness automation and analytics to eliminate inefficiencies, enhance compliance, and deliver measurable financial improvements from end to end.