Recover Lost Revenue through Smarter Appeals
Turn complex healthcare claims into financial opportunities. Neuriphy’s AI platform transforms medical documentation into tools for accurate, powerful revenue recovery.
Where Traditional Appeals Break Down
Documentation overload: Extensive notes, coding refs, and payer-specific formats eat time and invite errors.
Weak letter impact: Boilerplate appeals miss criteria and fail to meet payer expectations.
Coding checks are complex: Manual cross-checks of DRG assignments against payer criteria drain time and focus.
Resource heavy: Hours of chart review, validation, and letter drafting per case strain capacity.
Rules vary by payer: Different requirements and downgrade rationales create inconsistency and confusion.
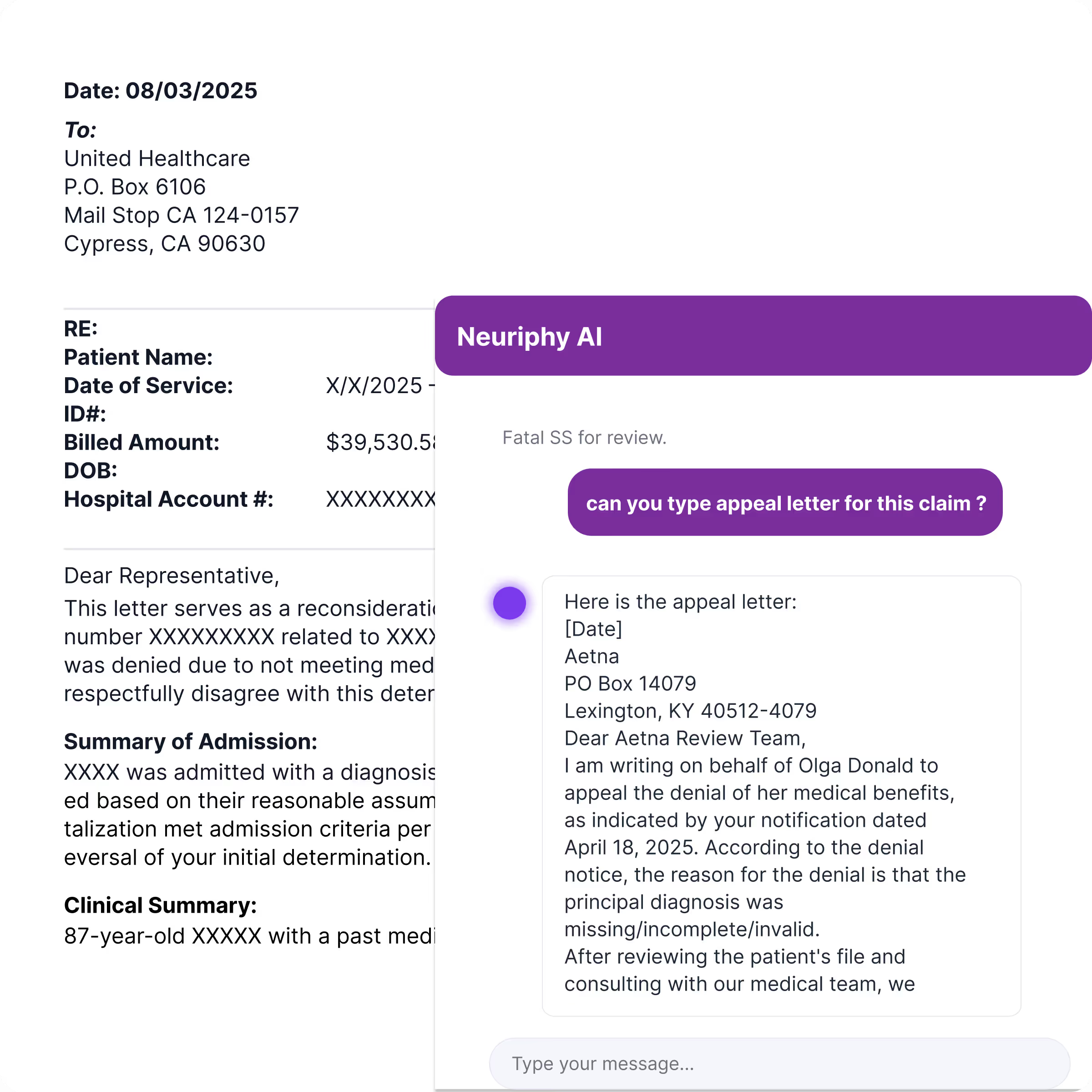
Stronger Medical Necessity Appeals
Automate case analysis, evidence gathering, and letter drafting to win more appeals, recover high-value revenue, and maintain compliance with payer and CMS rules.
Automated Case Analysis: Review denial reasons and map against payer-specific medical necessity criteria.
Intelligent Evidence Gathering: Extract the right clinical notes and coding references seamlessly.
Faster Appeal Drafting: Generate payer-ready, customized appeal letters in minutes.

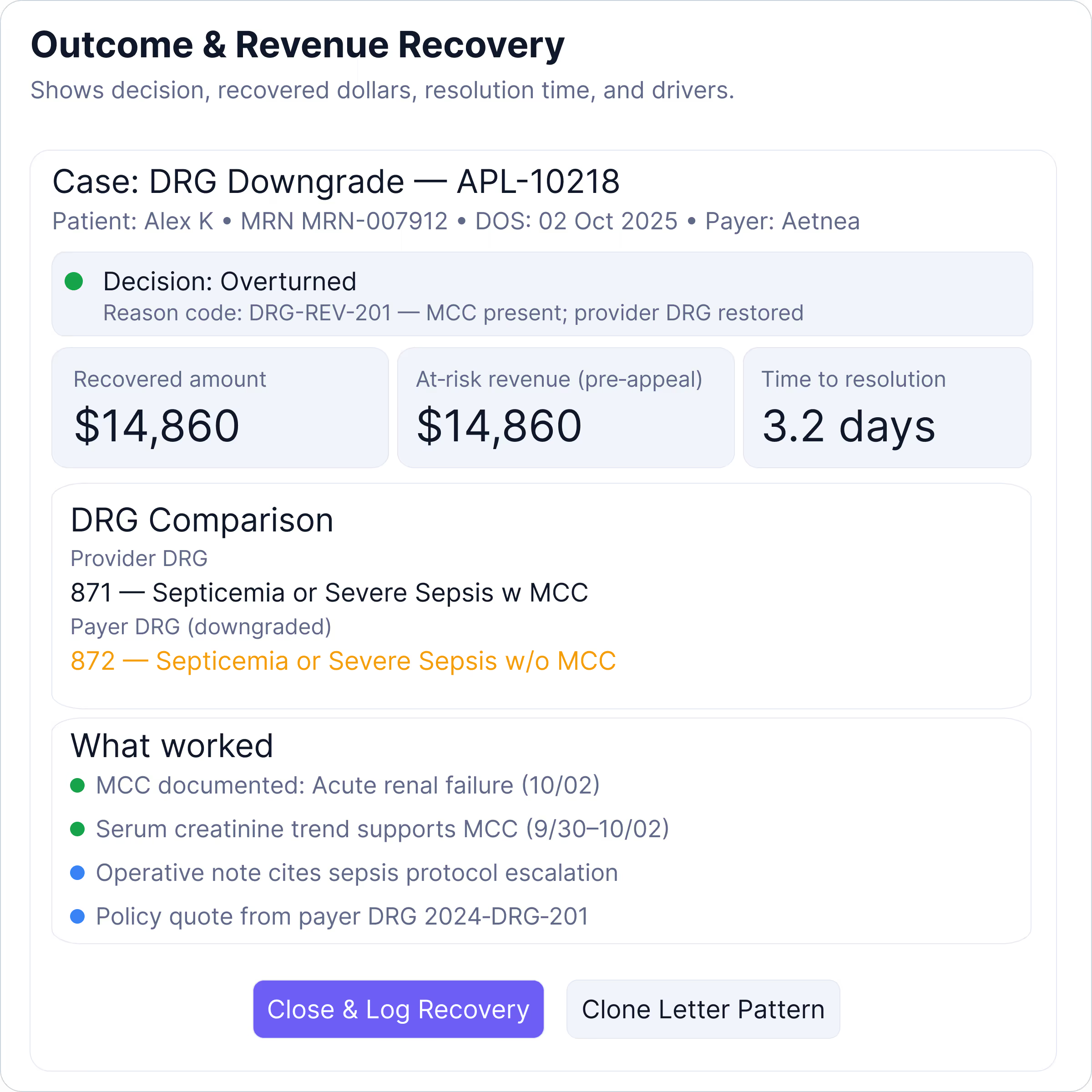
DRG Downgrade Appeals to Protect Hospital Revenue
Protect high-value reimbursements by validating DRG assignments, extracting supporting documentation, and drafting payer-specific appeal letters to overturn costly downgrades.
Automated DRG Validation: Compare provider-assigned DRGs with payer downgrades to flag discrepancies.
Evidence Extraction: Surface clinical notes, labs, and coding references for justification.
LLM-Powered Letters: Create audit-ready appeal letters aligned with payer rules.
Adaptive Appeal Strategies: Learns from payer responses and previous outcomes to continuously optimize DRG defense tactics.
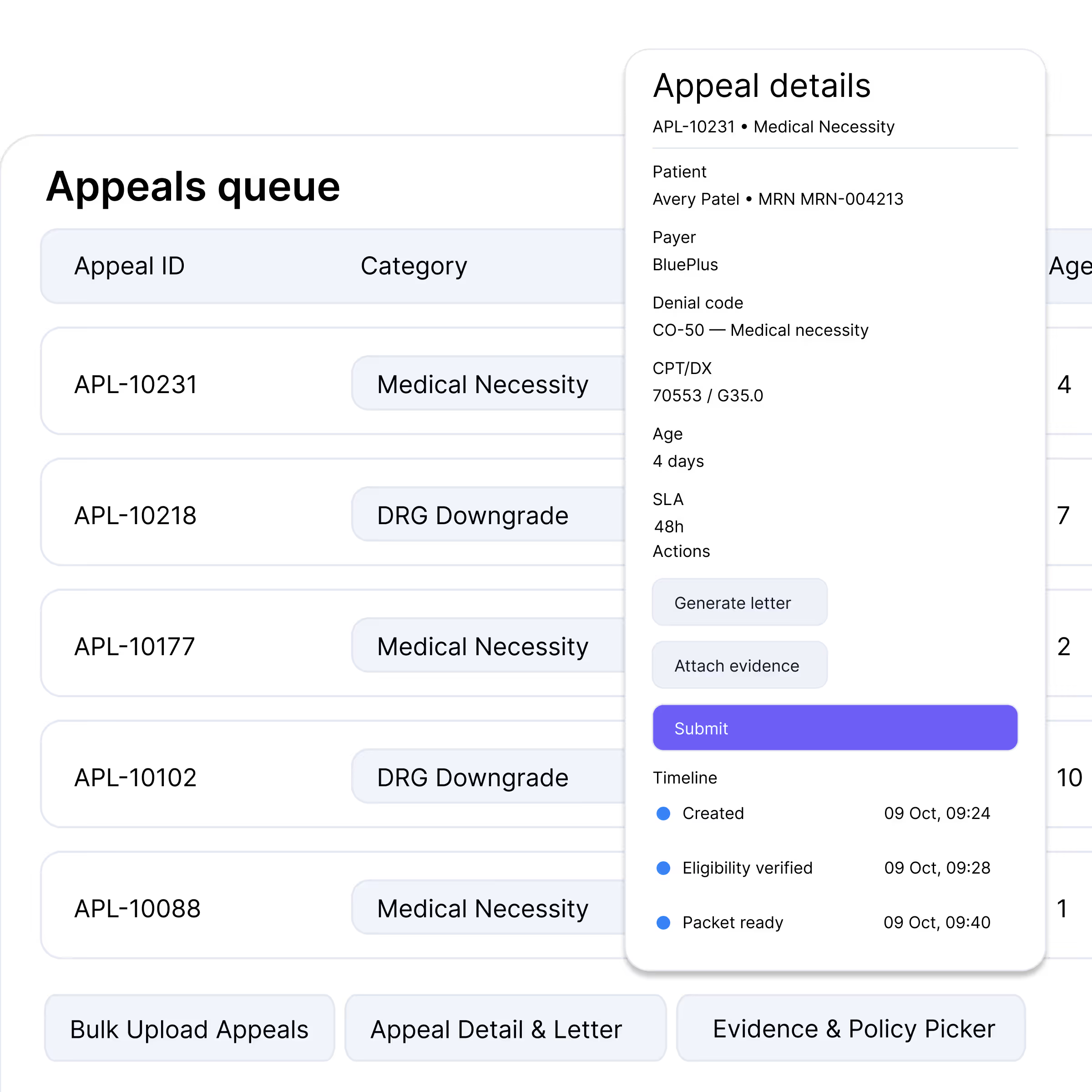
End-to-End Appeals Automation
From denial detection to payer-specific letter drafting, automate the appeals lifecycle for faster resolution, stronger overturn rates, and improved cash flow.
Denial Analysis: Map denial codes to payer-specific strategies and requirements.
Policy-Aligned Drafting: Generate narratives that match coverage rules and medical necessity standards.
Continuous Learning: Refine strategies by adapting to payer responses over time.
Evidence Packets that Strengthen Every Appeal
Our platform generates comprehensive clinical citations and evidence packets that transform complex medical documentation into compelling, actionable appeals.
Comprehensive Documentation: Compile medical records, coding references, and clinical notes into a unified, payer-ready packet.
Policy-Aligned Evidence: Match citations and guidelines directly to payer rules for stronger justification and overturn success.
Audit-Ready Format: Deliver structured, transparent packets that withstand payer scrutiny and regulatory audits.
Why Our LLM Makes the Difference
What differentiates our system is its foundation on a proprietary large language model tailored for healthcare revenue cycle management, setting it apart from standard AI tools.
Coding + clinical intelligence: Trained on DRG groupers, ICD-10/9 codes, and real clinical documentation.
Context-aware reasoning: Understands downgrade logic, adjusts to payer-specific standards, and drafts case-specific appeal arguments.
Learns continuously: Adapts to changing payer tactics and audit patterns.
Secure and compliant: HIPAA-ready foundation with enterprise-grade safeguards.
Impact of Smarter Appeals Management
Automated appeals workflows transform denial handling by improving overturn rates, accelerating reimbursements, and reducing manual effort—helping healthcare organizations secure more revenue with less operational strain.
Higher Overturn Success
Automated evidence packets and payer-specific letters increase appeal win rates and recover high-value reimbursements.
Recover High-Value Revenue
Protect reimbursement from downgrades that often reduce payments by thousands per case
Lower Administrative Burden
Automation reduces repetitive manual tasks, allowing staff to focus on strategic work instead of routine follow-ups.
Driving Measurable Results in Appeals Management
Our AI-driven platform delivers exceptional results in healthcare revenue recovery, converting complex financial challenges into strategic opportunities through intelligent automation.
Increased Win Rates
Reduced Operational Cost
Reduced Appeal Drafting Time
Kickstart Smarter Appeals Management
Learn how Neuriphy strengthens revenue cycle management through smart, AI-powered appeals processing that reduces denials and boosts recovery.