Streamline Patient Access with Our Proprietary LLM
Automate financial clearance from start to finish, accelerate eligibility checks, reduce errors, improve collections, and enhance the patient experience.

Where Traditional Financial Clearance Slows Care
Portal hopping: Staff juggle multiple payer sites and rules, interpreting dense policy language each time.
Error-prone details: Missing insurance info, wrong coverage status, and overlooked benefits trigger denials and rework.
Access delays: Clearance steps push out scheduling, procedures, and treatment start dates.
Financial exposure: Inaccurate eligibility leads to write-offs, bad debt, and surprise bills for patients.
Automated Eligibility Verification across Healthcare Networks
With high accuracy, Neuriphy’s AI platform automates eligibility and benefit verification, guaranteeing patients are cleared upfront, maximizing revenue while strengthening patient confidence.
Real-Time Checks: Instantly confirm patient coverage and benefits before service
99%+ Accuracy: Extracts and interprets complex plan documents, co-pays, deductibles, and prior authorization requirements.
Faster Workflows: Save staff hours with automation that clears patients upfront

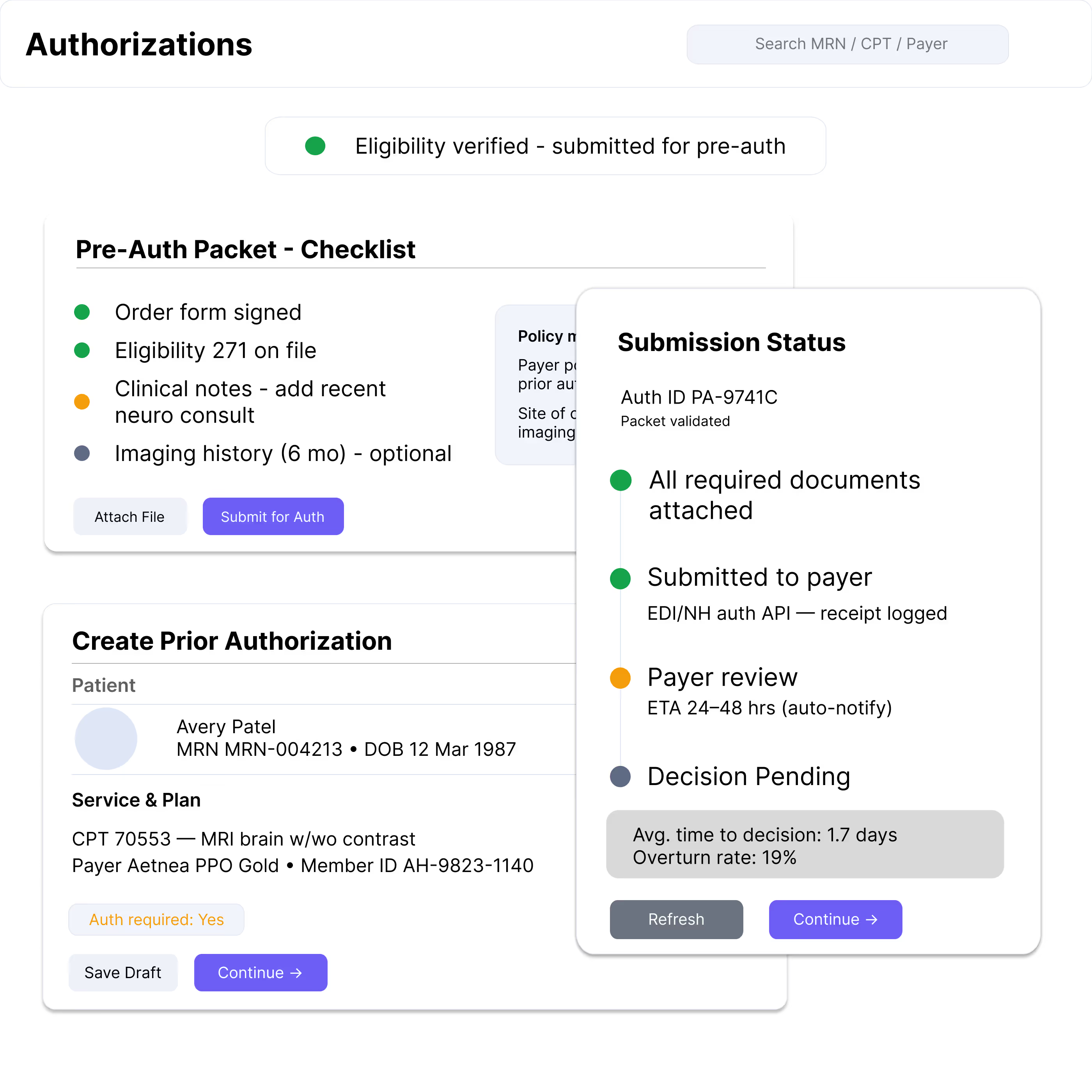
Pre-Authorizations Made Simple with Intelligent Workflows
Streamline approvals, cut delays, and reduce denials by automating pre-authorization tasks with smart, AI-guided processes.
Faster Approvals: Automate requests and reduce back-and-forth with payers.
Flags discrepancies in insurance data, expired policies, or mismatched patient details.
Efficient Workflows: Free staff from manual tracking and follow-ups.
Benefits of Intelligent Financial Clearance
Intelligent financial clearance improves patient access, reduces denials, and strengthens collections by automating eligibility checks, prior authorizations, and cost estimation with AI-powered precision.
Reduced claim denials
Eligibility errors and missing pre-approvals are caught early, preventing downstream denials and unnecessary write-offs.
Faster Patient Access
Instant eligibility verification and automated prior authorization workflows minimize scheduling delays and accelerate care delivery.
Stronger Collections
Accurate, patient-friendly cost estimates improve transparency, reduce bad debt, and support higher upfront payment rates.
Quantifying the Impact of Intelligent Financial Clearance
Claim Denial Reduction
Dramatic decrease in manual claim rejection rates
Payment Acceleration
Significant improvement in reimbursement speed
Operational Efficiency
Substantial reduction in administrative overhead
Transform Your Revenue Cycle Today
Take the first step towards intelligent financial clearance. Our experts are ready to show you how AI can revolutionize your healthcare revenue management.