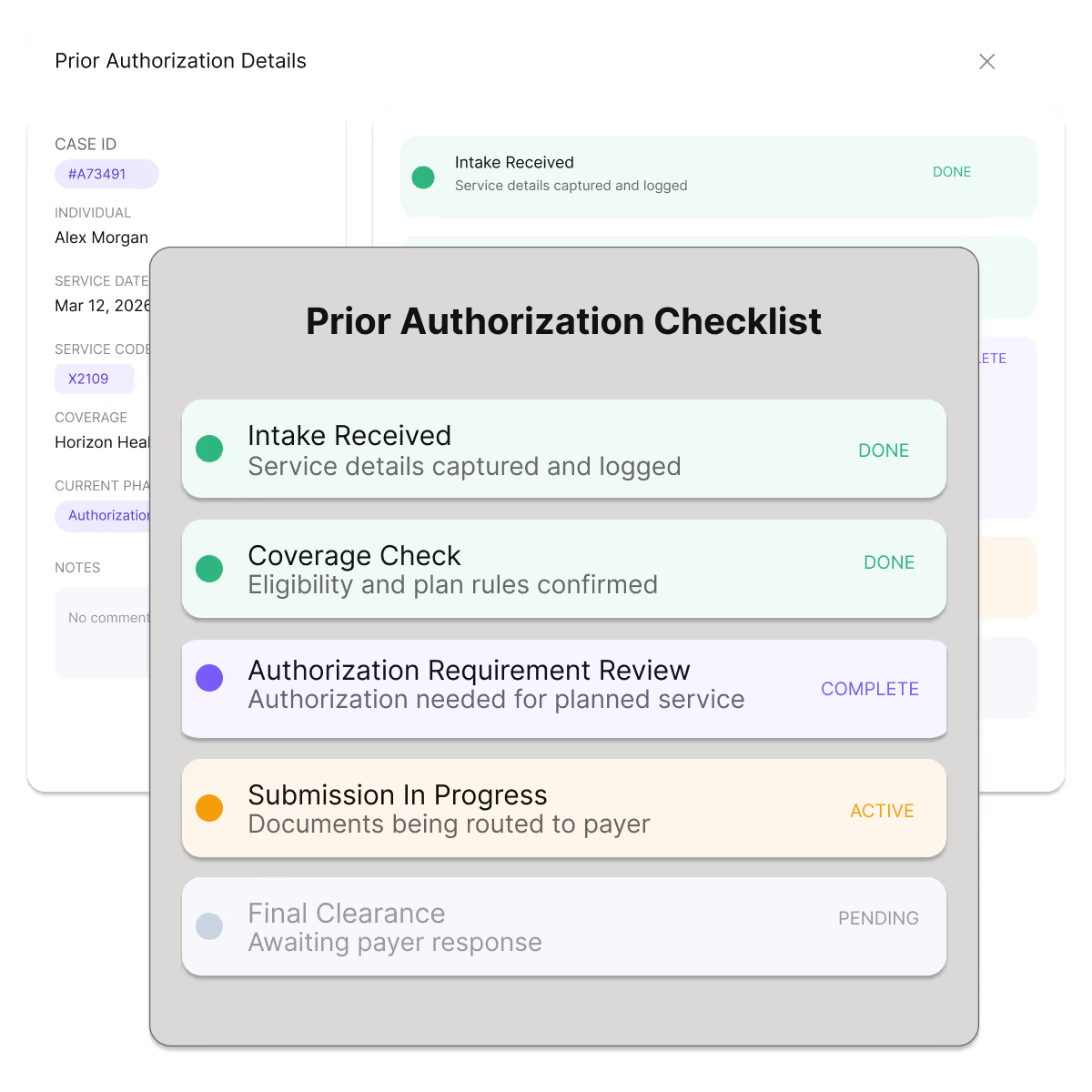
Prior Authorization, Automated End-to-End
Manage the full prior authorization process from requirements detection to submission and outcome tracking, with payer-aligned documentation and clear visibility that helps teams avoid missed deadlines, reduce rework, and improve first-pass success.

Why Prior Authorization Breaks Down
Hidden Authorization Requirements: Authorization rules vary bypayer, plan, procedure, and site of service—and change frequently—leading to missed requirements.
Manual Chart Chasing: Staff spend hours locating notes, imaging, labs, and prior therapies to meet medical necessity criteria.
Limited Status Visibility: Authorizations live across portals, faxes, and calls, making it hard to track progress or follow up on time.
Downstream Denials & Delays: Incomplete or late authorizations result in rescheduled care, denied claims, and poor patient experiences.
Authorization Requirement Detection
Neuriphy continuously evaluates scheduled services against payer rules to determine when prior authorization is required—and exactly what documentation is needed.
Matches CPT/HCPCS codes, diagnoses, and site of service to payer rules
Coverage-aware checks by payer and plan
Pre-service worklists prioritized by appointment date and risk
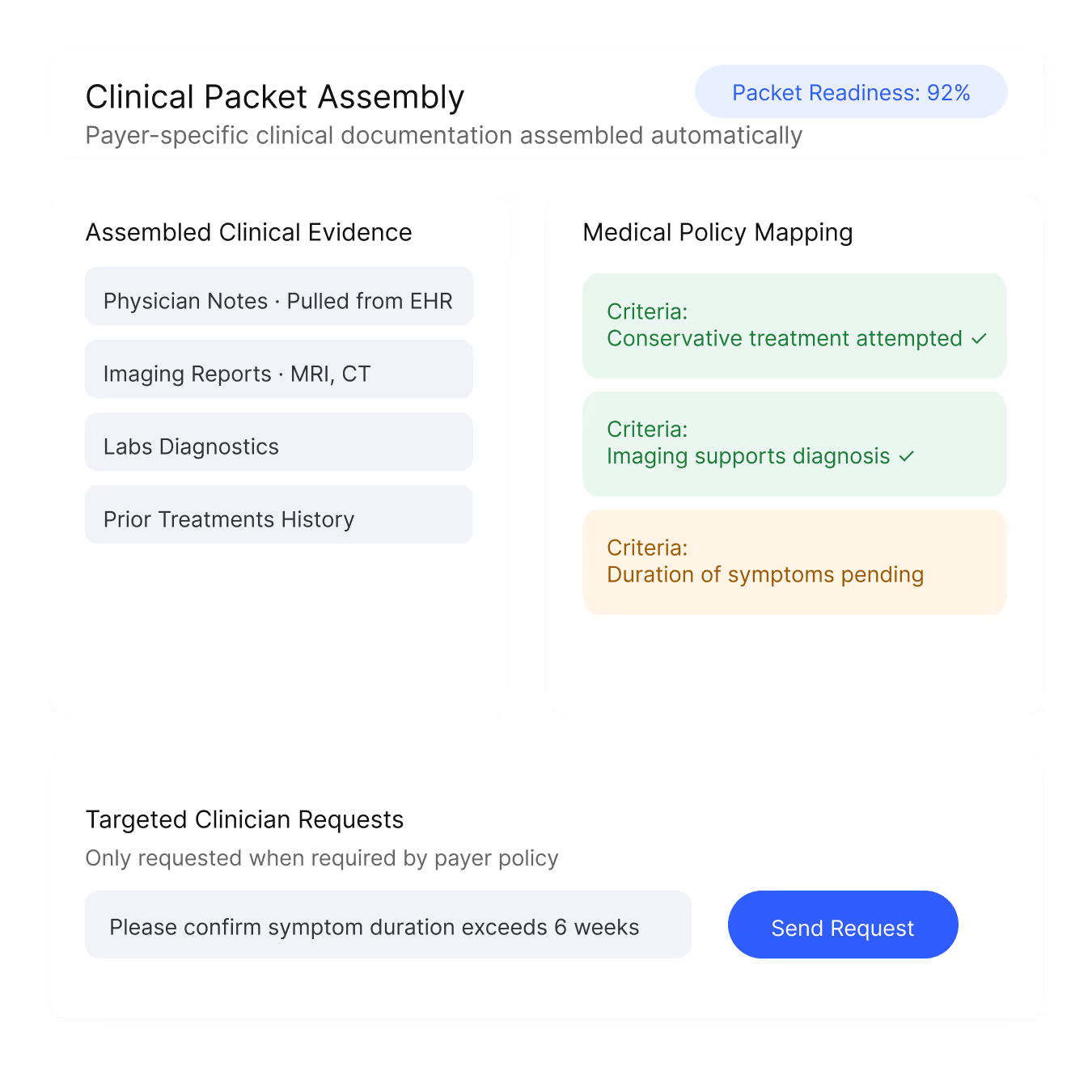
Automated Clinical Packet Assembly
Automatically assemble complete, payer-specific clinical packets—reducing back-and-forth and first-pass denials.
Pulls relevant notes, imaging, labs, and prior treatments from the EHR
Maps documentation directly to payer medical policy criteria
Generates targeted clinician requests only when information is missing
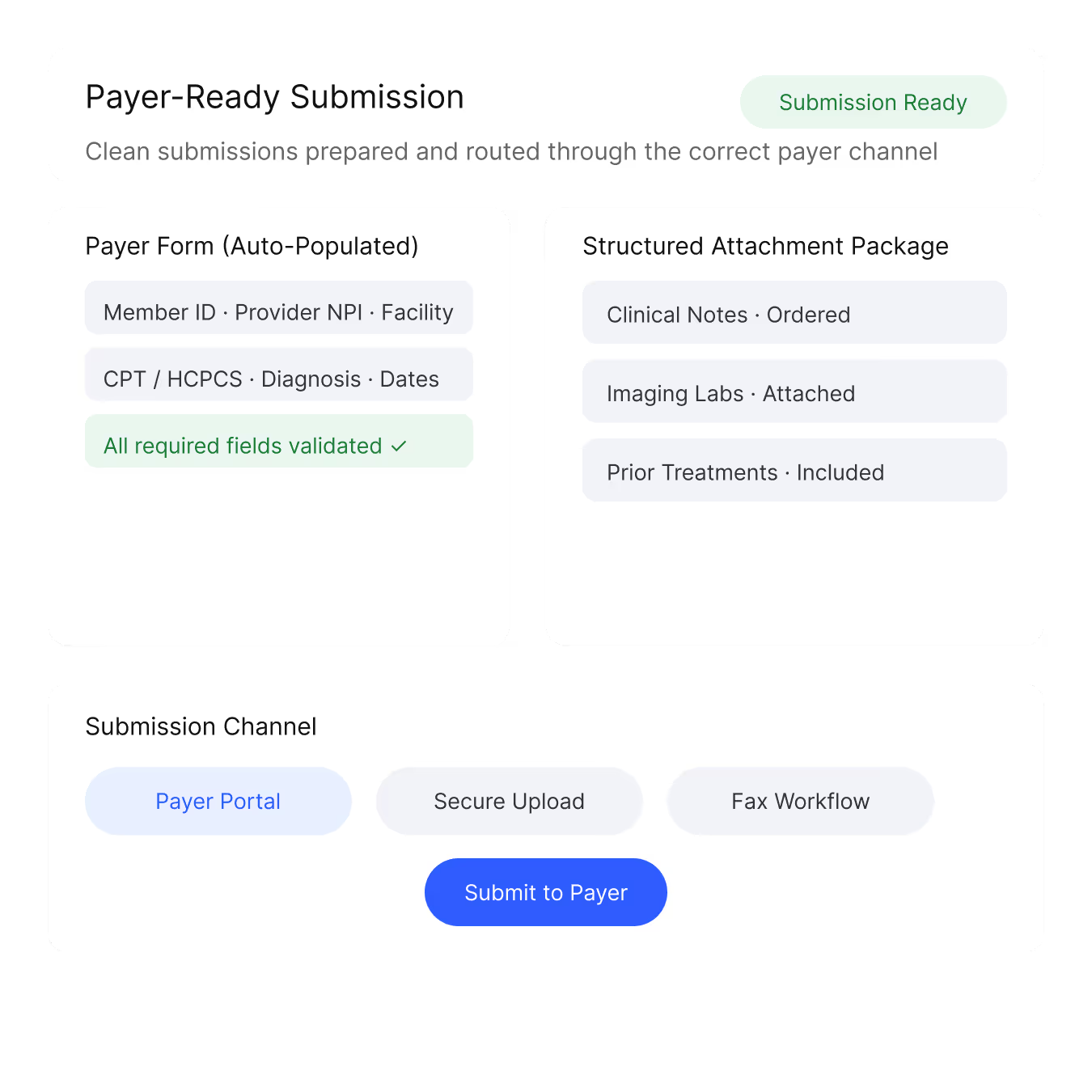
Payer-Ready Submission
Neuriphy prepares clean, complete submissions and routes them through the correct payer channel.
Auto-populated payer forms
Structured attachment packaging
Submission via payer portals, secure upload, or fax workflows
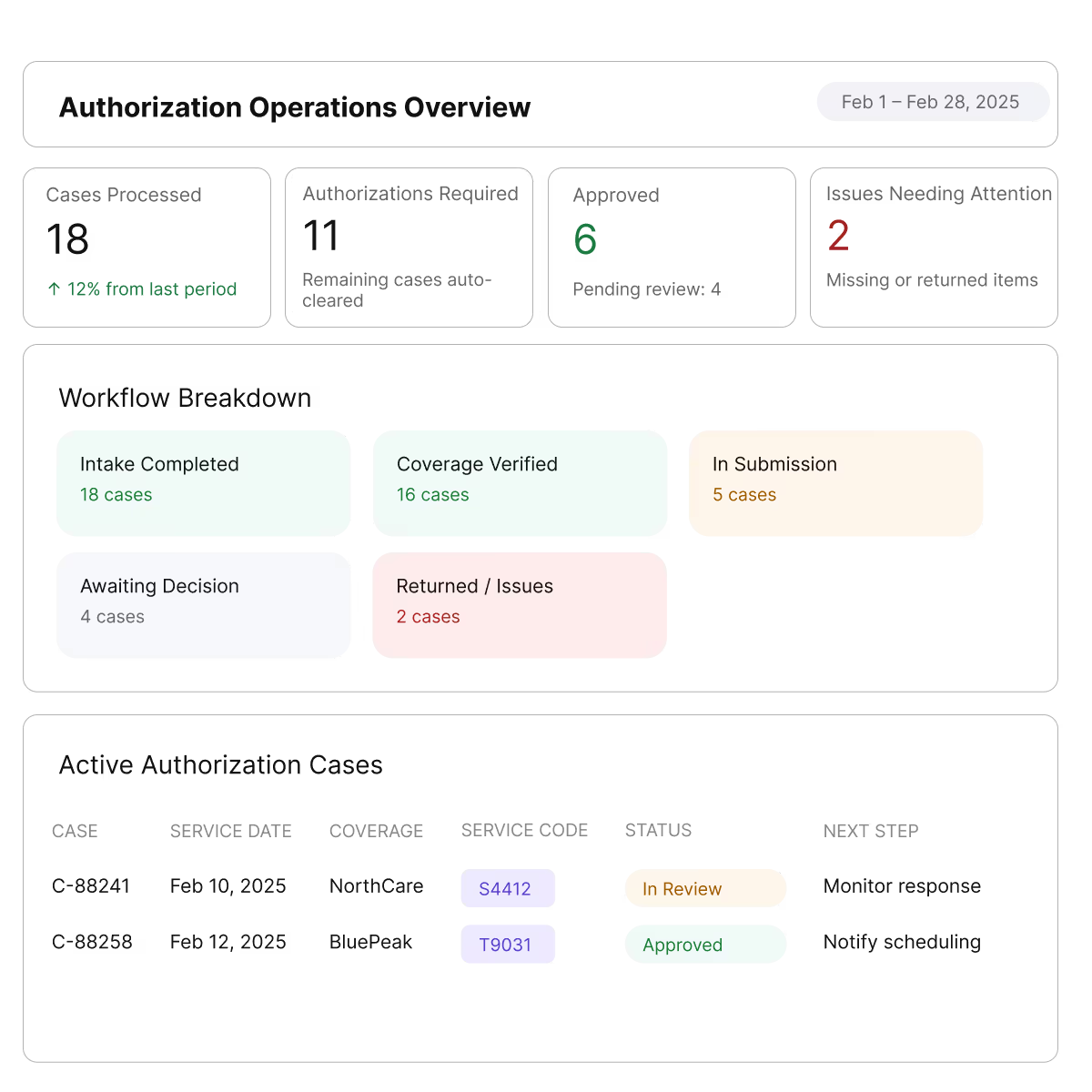
Real-Time Status Tracking & Follow-Ups
Eliminate “where is this authorization?” with centralized tracking and automated alerts.
Unified timeline of submission, pending, approval, or denial
SLA-based reminders and escalations
Clear updates for scheduling and patient access teams
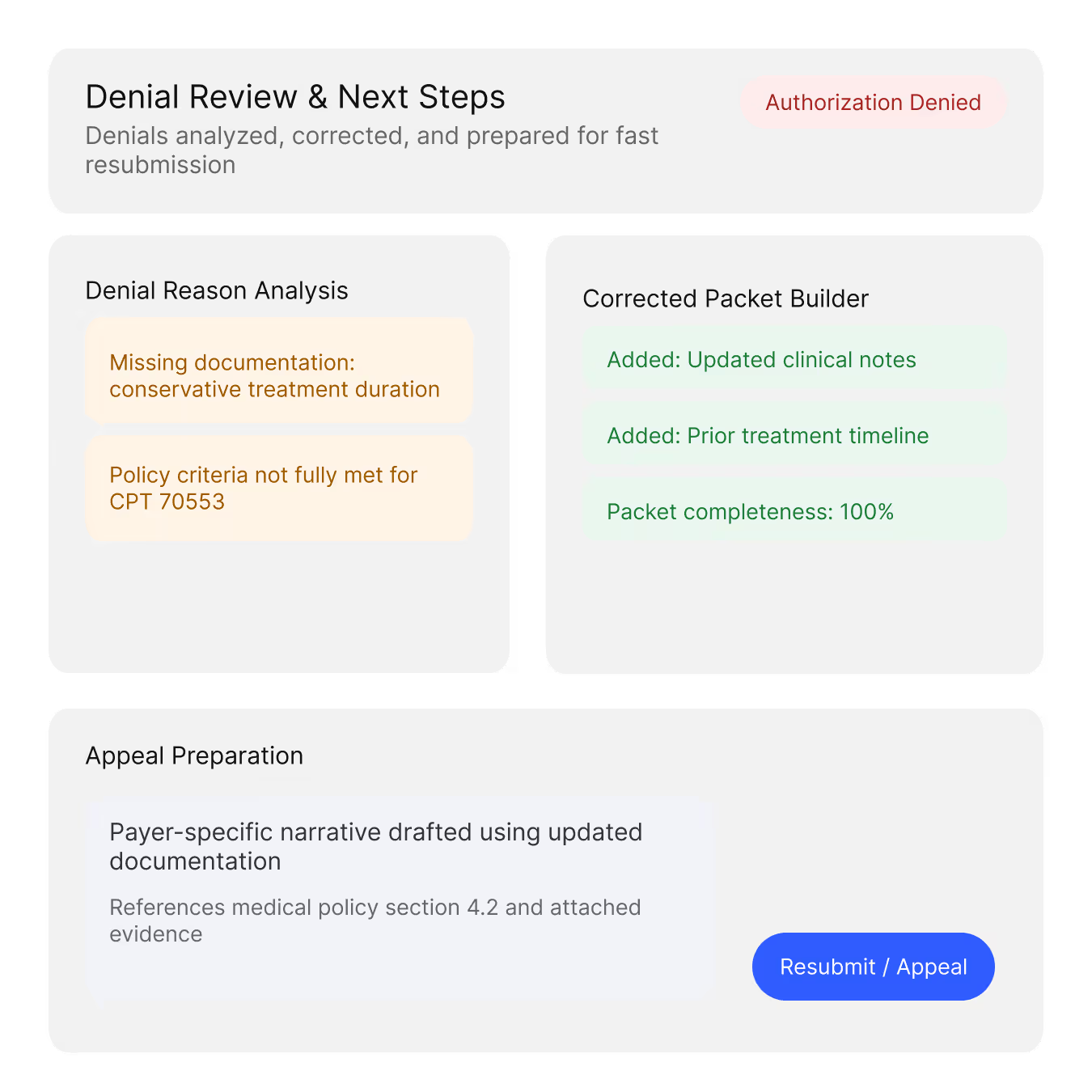
Fast Denial Resolution & Rework
When authorizations are denied, Neuriphy helps teams respond quickly with the right evidence.
Interprets denial reasons and missing criteria
Auto-builds corrected packets for resubmission
Supports appeal preparation with payer-specific narratives
What Sets Our System Apart
Healthcare-Specific Intelligence Engine
Purpose-built for revenue cycle operations, trained on payer policies, clinical language, and financial workflows.
Policy-to-Evidence Mapping
Connects payer medical policies directly to the exact chart evidence required for approval.
Closed-Loop Learning
Continuously improves based on outcomes—approval rates, turnaround times, and denial patterns.
Benefits of Smarter Prior Authorization
Clear decisions earlier. Fewer delays later. Stronger outcomes for teams and patients.
Fewer Delays in Care
Keep schedules intact.
Reduce rescheduled or postponed procedures caused by missing or late approvals.
Higher Approval on First Submission
Get it right the first time.
Improve first-pass approval rates with accurate, payer-aligned submissions.
Lower Operational Burden
Less follow-up. Less rework.
Cut manual effort, reduce downstream denials, and improve patient transparency.
Modernize Prior Authorization Today
Reduce delays, improve approval rates, and protect revenue—without adding staff.